What is the optimum age, if there is one, to have a child?
We know that fertility declines as time goes on - we've been told it takes something of a nosedive after 35 - so mother nature suggests younger is better. Yet, despite our early 20s being peak childbearing years biologically, better access to contraception, rising housing and living costs and the increasing number of women entering senior positions (we now make up one in three boardroom roles at 350 top UK firms) mean that each year we nudge the average age of first conception back a little bit.
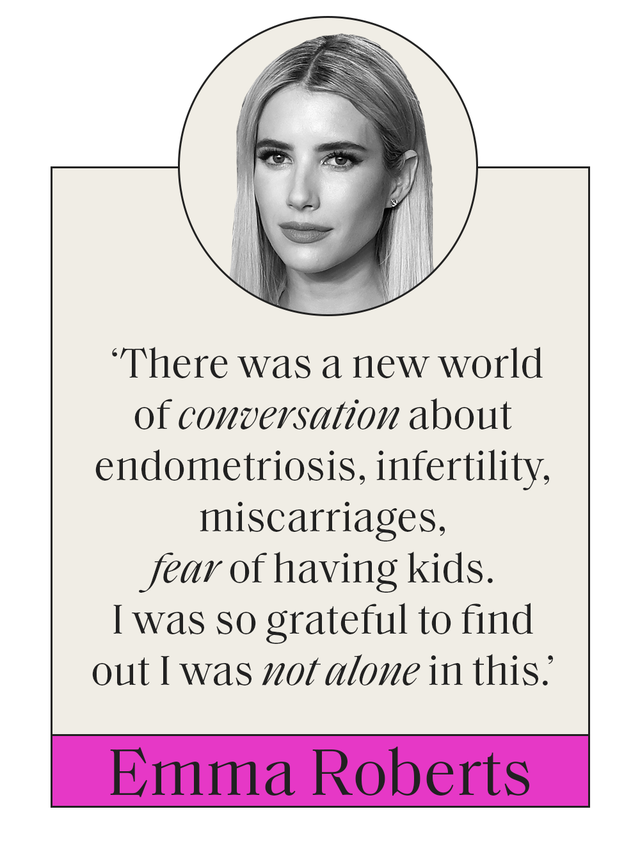
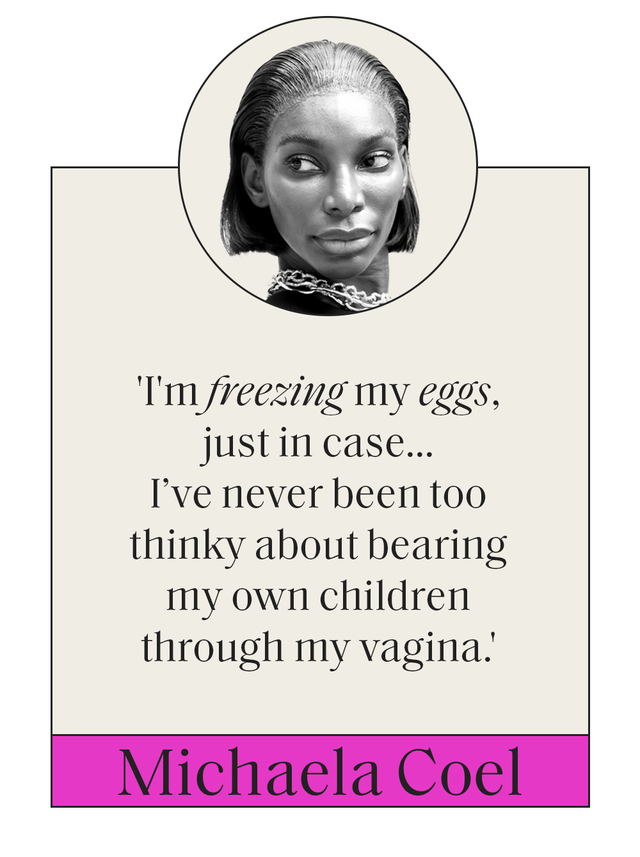
For these reasons and the mounting fear that a year of lockdown has pushed back our dating and procreating plans considerably, egg freezing is on the up and up.
In 2020, the UK's fertility regulator Human Fertilisation and Embryology Authority (HFEA) reported 2,377 egg freezing cycles in 2019, compared to 1,923 in 2018 (an increase of 23% and an increase of over 100% compared to 2015). And some clinics, like the fertility group Care Fertility, found that egg freezing enquiries had risen by 50% in November 2020, perhaps indicating that with so much time sat on the sofa under pandemic-induced house arrest, women have been craving ways to regain control over their futures.
‘Years ago nobody would mention that they were going to have IVF, because it was very personal,' Rachel Cutting, embryologist and the HFEA’s director of compliance, tells ELLE UK. ‘Whereas now there's more openness and acceptance, so young women talking about egg freezing is a more natural thing to do.’
When it comes to choosing whether or not you want to freeze your eggs, it’s important to know the facts. Let’s be clear - it is an expensive and physically demanding process. Age affects the success rate enormously and the storage time limit alone can result in some women not being able to use their eggs before they become inviable. ‘Egg freezing is not to be undertaken lightly,’ warns Cutting. ‘You're not guaranteed a baby at the end of it.’
We spoke to fertility regulators, embryologists and women who have frozen their eggs to find out more about the process and whether it’s worth your time, hopes and finances.
What is egg freezing?
Egg freezing does exactly what it says on the tin, so to speak. It’s a fertility treatment which involves collecting a woman’s eggs from her ovaries, freezing them and then thawing them at a later date.
As women’s chances of conceiving naturally decline with age – seven out of 10 women aged 30 will conceive within one year, compared to four out of 10 women aged 40 – so too does the quality and quantity of the eggs. Remember, women are born with all their eggs already in their ovaries and as they age, so do their eggs.
As a result, egg freezing is seen as one way of preserving a woman’s fertility so she can try to become pregnant at a point in the future, ideally removing eggs while a woman is young (i.e. at peak fertility) in order to collect eggs of the highest quality.
Liz Beardsell, creator and host of the sex and relationship podcast Diary, She Wrote, began freezing her eggs in 2018. It was during a brief relationship, aged 36, after being single for five years that she looked into the treatment. ‘Before that I hadn't really had a maternal desire,’ she tells ELLE UK.
‘But when I was dating my ex, I thought “Oh, actually, if I do meet the right person, then maybe I can see that sort of maternal desire growing”. I'm a really practical person and had savings, so egg freezing seemed like a sensible thing to do.’
And she's not alone in this thinking. According to the HFEA’s latest data, almost 53,000 patients had 69,000 fresh and frozen IVF cycles at the organisation’s licensed fertility clinics in the UK in 2019.
What does egg freezing involve?
Before a woman goes ahead with egg freezing, they must first be tested for infectious diseases, such as HIV and Hepatitis. It’s important to note that while these diseases don’t affect a woman’s eligibility to freeze her eggs, tests help inform medical experts whether some egg samples should be stored separately in order to prevent contamination.
‘What’s key for anybody considering IVF to know, is that it's not just a case of going and store your eggs – egg freezing requires a lot of time, commitment and several tests,’ notes Cutting, listing off doctor and nurses appointments, blood tests to check hormone levels, ovary scans and counselling sessions.
Following testing, the egg harvesting process begins, which involves a woman taking two types of medication – one known as down-regulation which suppresses the body's hormones to better control ovulation and another called a stimulation drug which boosts egg production and helps them mature. This means at least 10-14 days of hormone injections, up to three times a day, which a patient must administer themselves, in addition to regular blood tests at a clinic.
Beardsell describes the hormone injections as an ‘intense process’ and one that she wasn’t entirely prepared for. ‘It seemed so alien that the experts trust you with needles, to measure out the correct amount of medication, push air out of the needle, not get shards of glass into the medication after breaking its glass valve, and inject yourself at specific times of day,’ she says. From injecting herself at her work desk, to finding a wall outside her friend’s 30th birthday party venue to lay out her injection ‘kit’, it’s no wonder the podcast host recalls the process as ‘quite bonkers’.
When it comes to the injections, Cutting describes them as like ‘little diabetes pens’, adding that while they aren’t difficult to use, the process is a ‘commitment’. ‘You've got to carry the needles around with you, remember to administer the drugs at the same time every day and regularly visit your clinic to see how you're responding to the medication.’
Once the injection phase is complete, eggs will then be collected, vaginally, during a medical procedure whereby a woman will be placed under general anaesthetic or conscious sedation with pain relief. ‘A scanning probe is inserted through the vagina and a needle goes up to the ovary, where each follicle fluid sack is located. The clinician will then draw out the fluid to - hopefully - find an egg,’ explains Cutting. The entire process takes around 20-30 minutes and can result in mild period pain-like symptoms or more severe issues (noted below).
It’s common for about 15 eggs to be collected from a patient during this process, but it depends on numerous factors about the woman’s fertility, notes the HFEA.
Once this is completed, a cryoprotectant (more commonly known as a freezing solution) will be added to coat the eggs before they’re frozen, which is then done either by cooling them down slowly or by the more common, and increasingly more successful, process of vitrification (fast freezing, which involves storing them in liquid nitrogen at around -196 degrees Celsius in containers called dewars).
When a patient decides to use their frozen eggs, they will be thawed and those that have survived will then be injected with a donor's or partner’s sperm.
What’s the best age to freeze your eggs?
Deciding when to freeze your eggs is incredibly difficult, because it’s just not as simple as ‘the younger, the better’.
If you’re thinking about freezing your eggs, the HFEA states that it's best to do it before your 35th birthday. This is if you want the highest chance of success compared to trying to conceive naturally, particularly after the age of 40.
‘The most important thing to think about when you think of eggs is a woman's age,’ emphasises Cutting. ‘It's not the age of the woman when an embryo goes back into the body that's crucial, rather the age of the egg when it was collected.’
But in reality, the idea of collecting eggs from a very young woman and expecting her to be able to use them to become pregnant if she only feels ready many years later, is injudicious. In fact, the average age of women opting for egg freezing is 38. The majority of women prefer to freeze their eggs later in life for several reasons: the younger you are when you freeze your eggs the less likely you’re going to use them as you might conceive naturally and most women in their 20s and 30s don’t have the finances to freeze eggs in the first place.
Additionally, even if young women opt in, they might not be able to use their eggs by the time the 10-year storage limit expires (more on this below). For example, a 20-year-old who freezes their eggs would have to have used them by the age of 30 or risk them perishing. Recent data shows that the average age for first-time mothers in England and Wales is 28.9-years-old, with this stat creeping upwards year on year. So if you're freezing your eggs while very young, you really might not get to use them by the time you feel ready to take the leap.
How successful is egg freezing?
Before you freeze your eggs, it’s worth bearing in mind that the process does not guarantee success. While research and treatments are improving, only 18% of patients using their own frozen eggs in IVF treatment have a baby, according to the HFEA.
According to the Glasgow Royal Fertility Clinic, women who are under the age of 37 who freeze the recommended 15 to 20 mature eggs from multiple cycles have a 70 – 80% chance of giving birth to a child. This number declines to 65-75% for women aged 38-40 years old who freeze the recommended 25 to 30 mature eggs.
It will come as no surprise that using fresh eggs has a higher success rate than that of frozen eggs and embryos. ‘Egg freezing is an invasive procedure for an egg to go through. You need to hydrate, freeze, store and thaw the egg, which not all eggs can survive,’ Cutting explains.
However, as a result of vitrification technology, eggs are now much more likely to survive the thawing process (over 90% survival rate when the woman is under 35), according to Create Fertility. That said, the HFEA found that just 36 babies were born using the mother’s own ‘thawed’ eggs in 2016.
If you decide to freeze your eggs in your late 30s, when fertility and the success rates of an egg leading to pregnancies are already in decline, you may require more than one cycle of treatment to collect the eggs for storage. ‘That will be more invasive on your body, your life and, if you’re paying for treatment, your bank balance. But on the other hand, you are probably more likely to use your frozen eggs in the future,’ the HFEA notes.
If frozen eggs don’t lead to a pregnancy, IVF is still a possibility for those who are unable to conceive naturally (using fresh eggs), as is adoption.
When it comes to data regarding the success rate of egg freezing, Cutting warns that given the fact egg freezing makes up just 1.5% of IVF cycles currently carried out, there’s not enough verified data to provide accurate egg freezing success rate statistics yet. ‘A lot of eggs are being frozen, but not many have been used yet,’ she adds, alluding to the relatively new yet improving technology that’s used to carry out egg freezing. For example, while there were 2,377 egg freezing cycles in 2019, only 192 thaw cycles were carried out using patients' own eggs, which suggests that more patients are freezing eggs currently than thawing them to use in treatment.
‘It's important for patients to go and have counselling, talk to their doctor and try to find out realistically what their chances are because it might be less than 25% of having a baby at the end of it,' notes Cutting. 'It’s great to take control of your fertility, but you've got to be realistic about it.’
How much does egg freezing cost?
At present, the NHS only offers egg freezing to women for medical reasons, for example if they require an operation or treatment that could result in infertility, such as chemotherapy or radiotherapy. Transgender or non-binary individuals who are about to start hormone therapy or reconstructive surgery which might affect their fertility may also be eligible for NHS fertility funding.
The majority of women freezing eggs using NHS funding are aged below 35, with 89% below age 38. In 2016, the HFEA found that 81% of all egg freezing cycles were privately funded and 19% publicly funded. This changed from 74% private and 26% public in 2010.
The majority of women who opt for egg freezing pay for the treatment privately. The reasons for choosing this option – previously dubbed ‘social’ but now more commonly referred to as ‘elective’ – may include women wanting to freeze their eggs because they might not be in a relationship and want the possibility of conceiving naturally at a later date, or those who have fertility complications or are in the military.
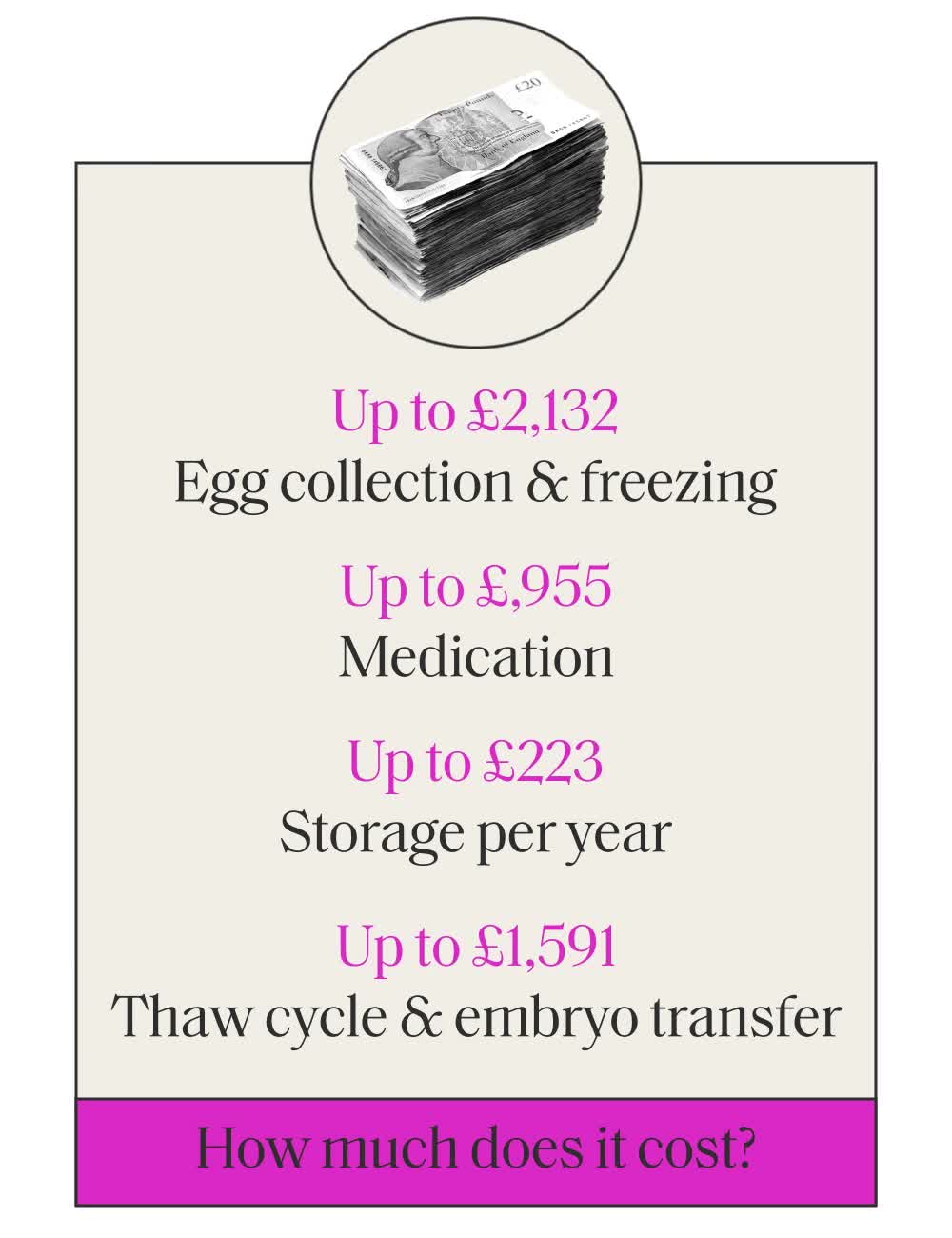
The cost of egg freezing varies but can cost from £7,000 to £8,000. Women can expect to pay up to £3,350 for the egg collection and freezing process. Medication can cost up to £1,500 and storage costs range from around £125 to £350 per year. The thaw cycle and embryo transfer costs an additional £2,500.
Melinda Mesiano, 30, tells us that she and her friends regularly discuss the possibility of egg freezing, but that she’s turned off by the eye-watering cost. ‘I’m not 100% sure if I want children, so, for me, I'd essentially be investing in the possibility of wanting children in the future. I’ve looked into it multiple times, but the cost is too high when you’re not certain,’ she admits. ‘On the flip side, I do worry that in 10 years’ time I will want kids and then it could be too late.'
Author and How To Fail podcaster Elizabeth Day has previously written about her experience of egg freezing process, describing it as ‘invasive and brutal’ and noting the true financial strain it can place on women. ‘One cycle cost £4,000,’ she wrote in You magazine in 2019. ‘That was before you factored in expensive fertility drugs and the £350 annual storage fee.
‘Every year, I now get a brutal reminder of time passing when the storage invoice lands on my doormat and I pay it off, wondering if I’ll ever get to a point where I want to use them and asking myself if I am emotionally strong enough to withstand the almost inevitable failure that lies ahead,’ she added.
In July 2020, former health secretary Matt Hancock said he was ‘instinctively open’ to the possibility of egg freezing being offered on the NHS to women aged 30 to 35.
In 2019 the investment bank Goldman Sachs began offering employees up to £15,000 under its ‘pathways to parenthood’ programme’ to cover the costs of egg extraction or purchasing donated eggs. The benefits were ‘designed to enable everyone in our workforce to better manage the commitment to their careers while starting, growing and supporting a family,’ a memo sent by the CEO David Soloman read. However, employees are expected to pay for long-term freezing and storage.
Cutting says that while this offer appears great on the surface, it’s not a solution to fertility. ‘It concerns me that the education is “Oh, it's fine, these companies will pay for you to have fertility treatment”,' potentially leading people to put off their family plans, 'But it's not a guaranteed success,' she finishes.
How safe is egg freezing?
Overall egg freezing is safe, but some patients experience side effects from the fertility drugs, which can range from mild discomfort to more severe issues.
The HFEA states that the main risks of fertility treatment are:
- a multiple birth
- ovarian hyperstimulation syndrome (OHSS)
- an ectopic pregnancy
- possible birth defects (the authority notes that this is rare and research is ongoing)
Multiple births:
It might be odd to think of multiple births as a serious health issues, but according to the authority, having more than one baby can cause serious harm to the health of mother and child, with at least half of twins born premature and underweight. ‘You’re also more likely to have an early or late miscarriage if you’re carrying multiple babies,’ the HFEA states.
When it comes to mothers, multiple births can result in high blood pressure, gestational diabetes, anaemia and occasionally haemorrhage. It is possible to reduce a woman’s chances of having a multiple birth if they choose an elective single embryo transfer (eSET), which involves transferring just one embryo into the womb instead of several as was previously common. All remaining embryos can be frozen and be used at a later date.
It’s worth noting that eSET doesn’t affect egg freezing’s success rate, but it’s not suitable for everyone.
Ovarian hyperstimulation syndrome (OHSS)
This is a reaction to the fertility medication and usually occurs around a week after egg collection. OHSS happens when a woman is hypersensitive to the drugs and develops too many eggs in the ovaries, which can result in them becoming enlarged and painful.
Approximately a third of women will suffer from mild OHSS, which can vary from nausea and vomiting, stomach pains or faintness and can normally be treated at home with pain relief. However, anyone who is suffering from strong symptoms is advised to contact their clinic immediately. ‘Never feel you are wasting the clinic’s time,’ notes the HFEA.
Ectopic pregnancies
An ectopic pregnancy occurs when a baby develops outside of the womb, commonly in the fallopian tube. If a woman is experiencing an ectopic pregnancy then medical help is required as the pregnancy can no longer proceed and a failure to address the issue could result in a rupture of the fallopian tube and internal bleeding.
While all pregnant women are at risk of ectopic pregnancies, those who have had IVF may be more at risk due to the process of the embryo being transferred to the womb as it could travel to the fallopian tube instead.
Symptoms of an ectopic pregnancy include a one-sided low abdominal pain, vaginal bleeding and diarrhoea or pain when going to the toilet.
Birth defects
It’s unknown whether birth defects may come as a result of fertility treatment or fertility issues in parents, but there is research to suggest that fertility treatment like egg freezing could be linked to an increased risk of birth defects, however these are ‘very low’ according to the HFEA and shouldn't necessarily affect your decision to choose egg freezing.
How long can eggs be stored for?
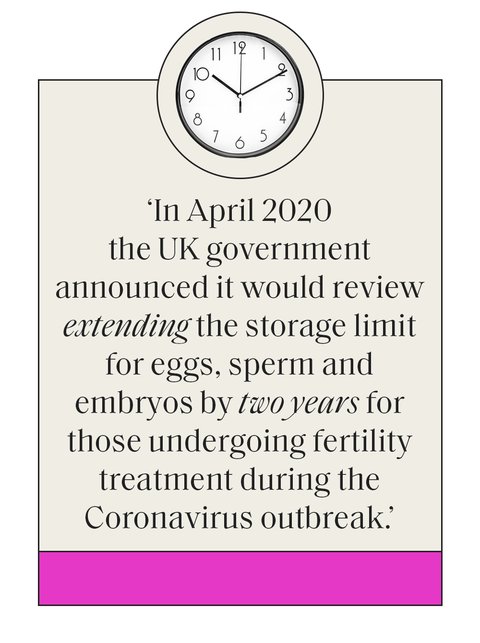
On average, eggs can be stored in the UK for up to 10 years, but in some cases, such as if the patient became prematurely infertile due to medical treatments, some might be able to keep them frozen for up to 55 years.
In April 2020 the UK government announced it would review extending the storage limit for eggs, sperm and embryos by two years for those undergoing fertility treatment during the Coronavirus outbreak so that they have more time for treatment. After all, the current limit was decided in law over 31 years ago.
In the lead up to the review announcement, the Royal College of Obstetricians and Gynaecologists (RCOG) said that the 10-year storage limit may discourage women from freezing eggs in their 20s, opting instead to do it in their 30s, when the quality of their eggs is reduced. ‘If she is not ready by the 10-year limit, she will then have to decide whether to become a parent before she is ready, transfer her eggs to a fertility clinic outside of the UK if she can afford to do so, or have her eggs destroyed,’ the organisation noted.
The HFEA has described the current limit as ‘too restrictive’ and proposes several conditions, including the patient providing new written consent to storage every 10 years (up to a maximum of 55) and that a clinic offers the patient counselling before they consent to every additional 10 years storage.
Regardless of limit, it’s important a woman keeps their clinic up to date with their change of address and contact details as if it’s unable to reach you at the end of the 10-year consent period, it might have to remove your eggs from storage.
What happens if you decide to use your eggs?
If a woman decides to use their eggs they must contact the clinic and discuss the thawing process. Thawed eggs must be fertilised using a treatment known as Intracytoplasmic sperm injection (ICSI) as the freezing process strengthens the coating around the eggs and makes it harder for sperm.
There are also several options if you’ve frozen your eggs and don’t want to use them. You can donate them to research to help the medical community look further into infertility and treatments, donate them as samples for trainee embryologists to practice different techniques, or donate them to another person.
You can also choose to discard them, which will involve the removal of the eggs from the dewars and allowing them to ‘perish’ in warmer temperatures. ‘What we've seen, and what's in the literature, is that many women who do freeze their eggs will never go back and use them,’ says Cutting.
To find out more information about egg freezing and how to start the process, contact the HFEA here and find a clinic here.

Katie O'Malley is the Site Director on ELLE UK. On a daily basis you’ll find Katie managing all digital workflow, editing site, video and newsletter content, liaising with commercial and sales teams on new partnerships and deals (eg Nike, Tiffany & Co., Cartier etc), implementing new digital strategies and compiling in-depth data traffic, SEO and ecomm reports. In addition to appearing on the radio and on TV, as well as interviewing everyone from Oprah Winfrey to Rishi Sunak PM, Katie enjoys writing about lifestyle, culture, wellness, fitness, fashion, and more.